Malignant Syphilis: A Rare Case of Early Secondary Syphilis in an Immunocompetent Patient

Malignant syphilis, also known as lues maligna, is an uncommon and aggressive variant of secondary syphilis. It is most often reported in individuals with compromised immunity, particularly those living with HIV. However, rare cases have been documented in immunocompetent patients, making diagnosis challenging and frequently delayed.
This condition represents an exaggerated inflammatory response to Treponema pallidum, leading to severe systemic and cutaneous manifestations that differ from classic secondary syphilis.
Clinical presentation
In immunocompetent patients, malignant syphilis typically begins abruptly. Symptoms often include high fever, malaise, weight loss, headache, and muscle or joint pain. These systemic features may precede or accompany skin findings.

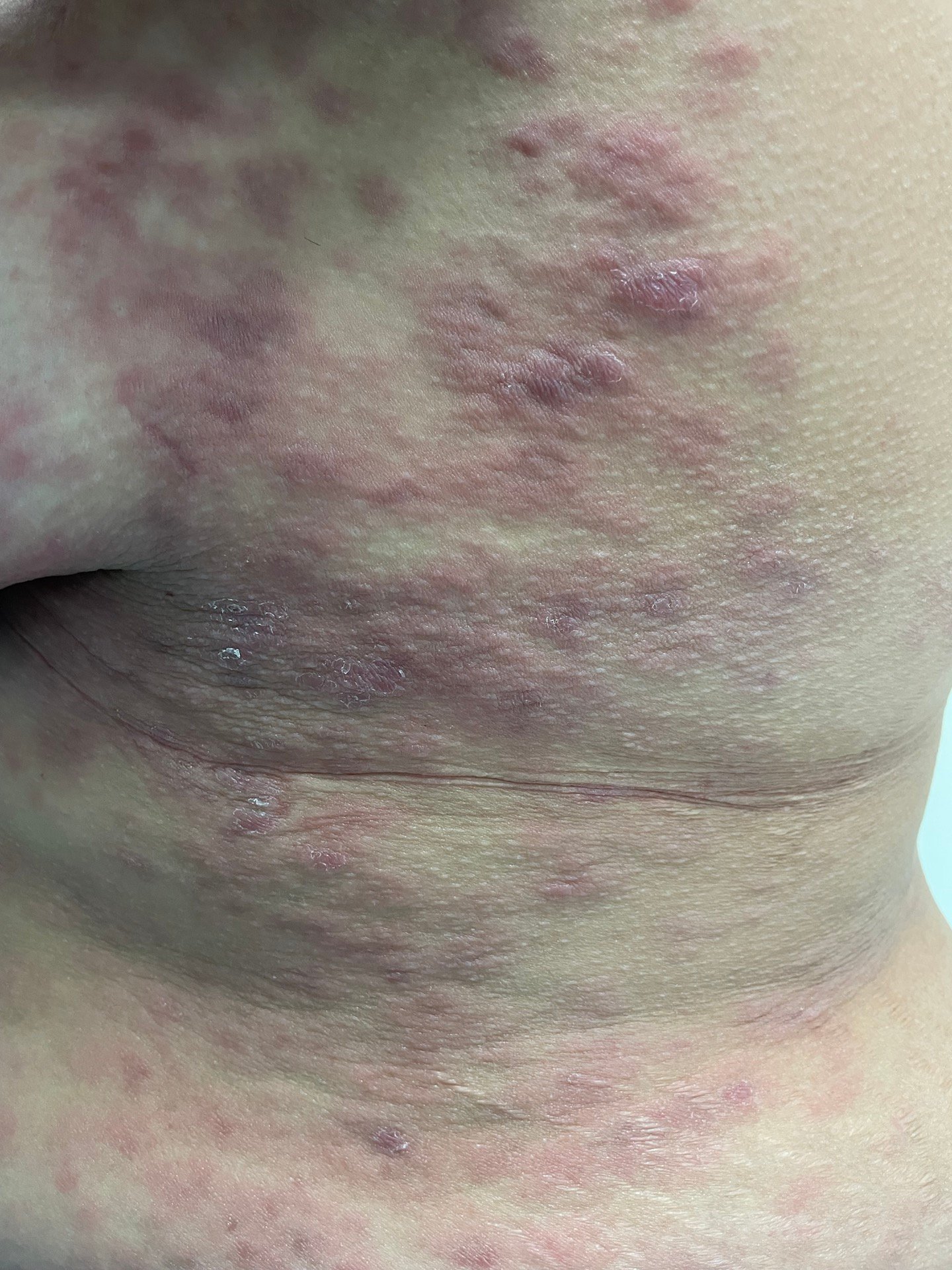
Cutaneous lesions are the most striking feature. Patients develop multiple painful papules or nodules that rapidly ulcerate, forming deep necrotic ulcers covered with thick, dark crusts. These lesions may resemble vasculitis, deep fungal infections, pyoderma gangrenosum, or even cutaneous lymphoma, which frequently leads to misdiagnosis.
Unlike typical secondary syphilis, mucous patches and generalized lymphadenopathy may be minimal or absent.
Diagnosis
Diagnosis relies on a combination of clinical suspicion, serologic testing, and histopathology. Non-treponemal tests such as VDRL or RPR are usually strongly positive, with high titers. Treponemal tests confirm the diagnosis.
Skin biopsy often reveals dense dermal inflammatory infiltrates rich in plasma cells, endothelial swelling, and necrosis. Spirochetes may be scarce on special stains, which can complicate confirmation. Importantly, HIV testing is essential, even when patients appear immunocompetent, due to the strong association.
Pathophysiology
The exact mechanism behind malignant syphilis in immunocompetent individuals remains unclear. It is believed to involve a hypersensitivity reaction to T. pallidum, resulting in severe tissue damage. High bacterial load and delayed immune regulation may also contribute.
Treatment and response
Despite its alarming presentation, malignant syphilis responds well to standard syphilis therapy. Intramuscular benzathine penicillin G remains the treatment of choice. Patients often experience a rapid clinical improvement after therapy, although a Jarisch–Herxheimer reaction is common and may be severe.
Lesions gradually heal over weeks, often leaving residual scarring or hyperpigmentation. Follow-up serologic testing typically shows a significant decline in non-treponemal titers.
Clinical significance
This rare presentation highlights the importance of considering syphilis in the differential diagnosis of necrotic skin ulcers, even in patients without immunosuppression. Early recognition prevents unnecessary investigations, inappropriate treatments, and long-term complications.
Malignant syphilis, though uncommon, remains a reminder of why syphilis continues to be known as “the great imitator” — capable of surprising clinicians even in modern medical practice.